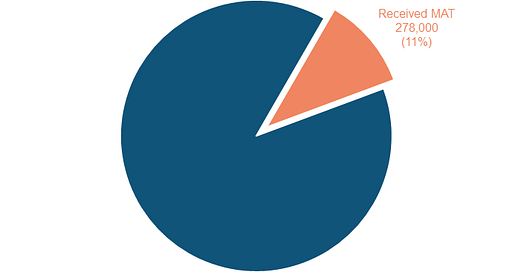
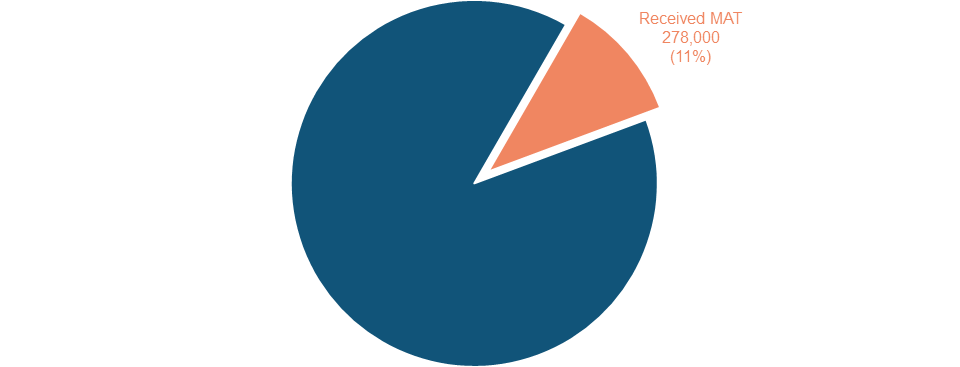
Out of 2.5 million people in this country with opioid use disorder, a chronic condition with an annual mortality rate of 10%, only 278,000 (11%) are receiving treatment. Consider this: For every patient in Medication Assisted Treatment (MAT), there is one other person who dies.
In 2020, only 10% of primary care physicians had the "X-waiver" to be able to prescribe buprenorphine for substance use disorder. This requirement has now been dropped (although electronic medical records generally have not yet been updated to make this possible for doctors without such a waiver). But in 2020, only 24% of those who had the waiver actually used it to prescribe buprenorphine.
So, how do we get more people into treatment?
Under the waiver restrictions, buprenorphine prescribers were limited in how many patients they could treat, depending on how long they had been qualified and whether they worked in a substance abuse clinic. Back then, many clinics tried to build a "hub and spoke" model, where patients would get induced and stabilized in the hub and then transition out to their primary care provider to continue treatment. But community providers were reluctant to take on these patients. I heard worries about the "clientele" disrupting the waiting room and other such prejudices.
So, even with the waiver gone, I hold little hope that primary care practices that don't have their own clinics will welcome even stable buprenorphine patients for this part of their continued recovery.
I think those of us who treat opioid use disorder, the most realistic way to move forward is to try to find ways to take on more patients. But there are restrictions, imposed by insurers, Medicaid in particular. You have to have a certain number of therapists in the recovery group depending on the number of participants, and in order to pay the doctor for prescribing and overseeing the medical aspect, there has to be a face-to-face encounter. And you can only do so many in whatever time your group is scheduled for - in my case 90 minutes.
But, strictly speaking, other reimbursement mechanisms may be available. There are grant monies that could move us away a little bit from the face to face with the prescriber and, just like in other areas in medicine, there could be scribes. We also have peer counselors and medical assistants who can gather information, do drug tests and so on.
As much as I enjoy and value the therapeutic aspects of my long term relationships with relatively stable MAT patients, I am starting to feel that maybe I could see them less often in order to make room in my schedule for new patients. Given the fentanyl crisis, and given the statistic that as soon as an addict enters a MAT program, their risk of dying from an overdose drops by 38-59%, perhaps we are not using ourselves as a resource in the most efficient way possible. After all, we are in a crisis. Are we in enough of a crisis mode for the situation we are in?