I have one patient in each of my clinics with a long history of relentless abdominal pain, mild constipation, poor appetite and general malaise. Neither one has any abnormality on any of the testing I or my colleagues at the clinic or in the nearest hospital have done: An alphabet soup of blood tests, CT scans, ultrasounds, endoscopies, gastric emptying studies and I don’t know what.
Each one of these older gentlemen usually comes in looking pale and gaunt, saying “I just don’t feel good, Doc”.
Now, one of them seems to be cured, within three days of starting a new prescription, intended to treat something else.
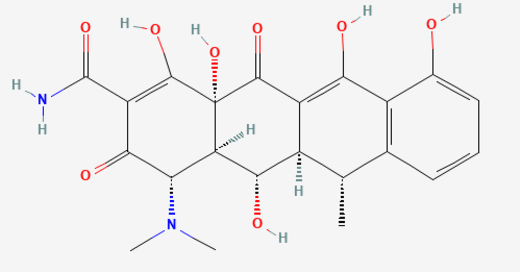
Hector Dunn happened to come in with a COPD exacerbation within a couple of months of his last one. I prescribed the usual steroid, but, because it hadn’t been too long since he had taken the usual Bactrim, I put him on doxycycline.
When I saw him in followup, my medical assistant warned me: “You’re not going to believe this, but Hector looks and feels like a million bucks”.
I knocked on the door of his exam room and entered.
He jumped out of his seat, grinned and gave me a strong, firm handshake.
“I feel better than I’ve felt in years after that last prescription. My breathing got better right away, but my stomach feels great, I don’t hurt anywhere and I have all kinds of energy. I’d say I feel the best I have felt in twenty years.”
His wife nodded and chimed in:
“The day after he started the doxycycline, he got rid of all kinds of gas over about 48 hours, and then he was like a new man.”
I sat quietly and took in the scene before my eyes and, just like with the patient I once had hat developed Parkinson’s disease under my nose and was diagnosed and treated by someone else, I suddenly saw Hector move his face while he talked, shift forward in his chair, make gestures with his hands, arms and shoulders as he provided more vivid and extraneous details about his colonic gas elimination. I had never seen him that lively; before that, he had always carried himself as if any extra effort or movement might cause him to crump.
“Could that antibiotic have gotten rid of some intestinal infection he had been carrying for years”, his wife asked, astutely.
“Absolutely”, I answered. “It’s called SIBO, or Small Intestine Bacterial Overgrowth. While we are supposed to have billions of bacteria in our large intestine, the small intestine should not have bacteria in it. Sometimes it does, and that can cause anything from diarrhea to chronic abdominal pain and bloating, and I now have to admit that may have been what Mr. Dunn has had for a long time now. There’s no handy test for it so sometimes we just guess and treat, but it had not occurred to me. Doxycycline isn’t the typical treatment for it, but it can work, and doxycycline also has some antiinflammatory properties, and SIBO may have elements of inflammation linked to it.”
“I don’t know what any of that really means, but I do know I feel good”, Hector concluded, rose from his chair and patted me on the shoulder. He seemed eager to get out of there, unlike other times when I was probably the one who wanted the visit to end because of my own helplessness.
“Now, I’ll need to hear if the belly pain comes back”, I said. If it does, we’ll have to decide if we’re going to use doxycycline again, or the stuff the books say might work even better. Let me know how you’re doing, okay?”
Later that day, I thought about my other patient, Percy Barr. What if he might respond to doxycycline, too? But he’s on warfarin, and there’s an interaction between those two drugs. I’d probably give him rifaximin. But he’s in Florida, as every other winter.
So in a twist of fate, I’m starting to look forward to him coming back, now that I have something different, new and promising to offer him.



Thank you!